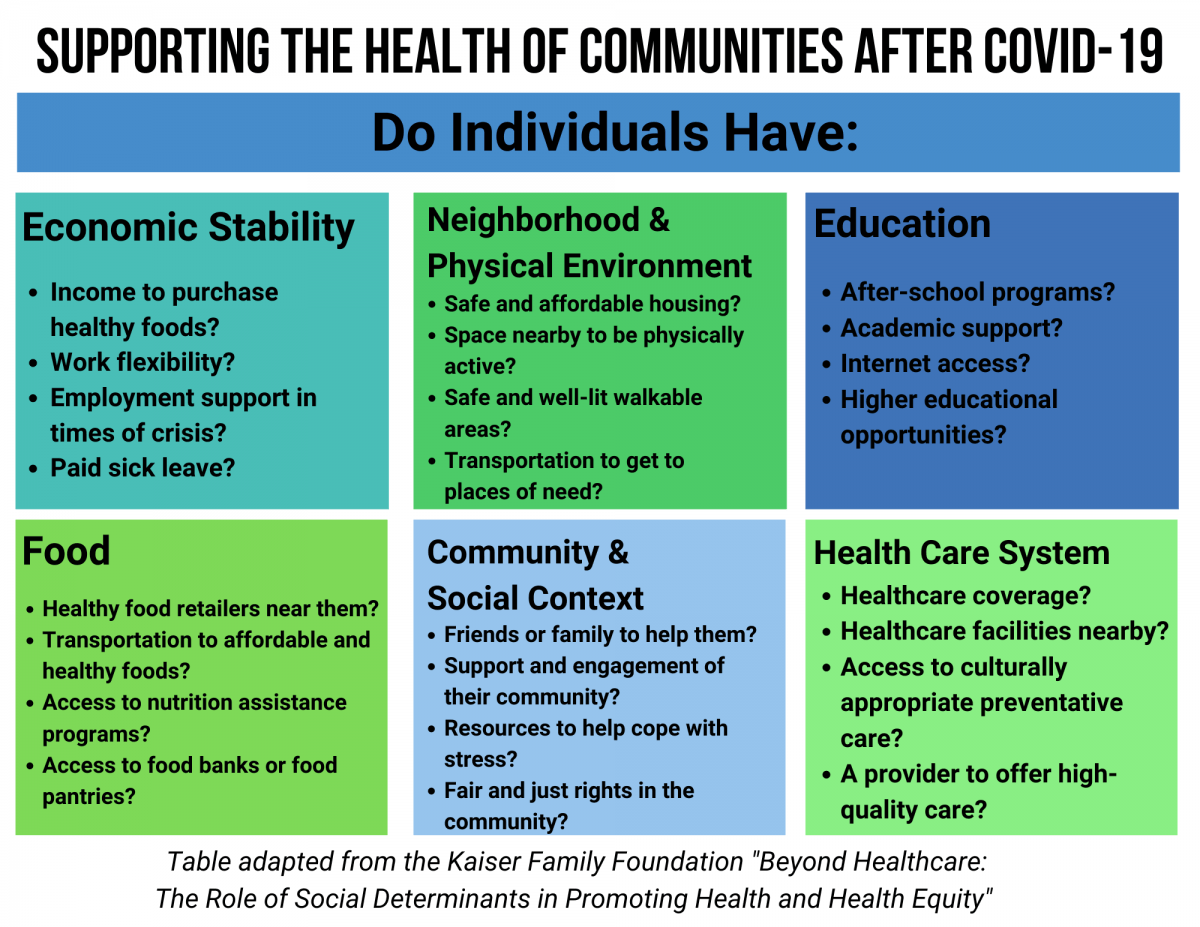
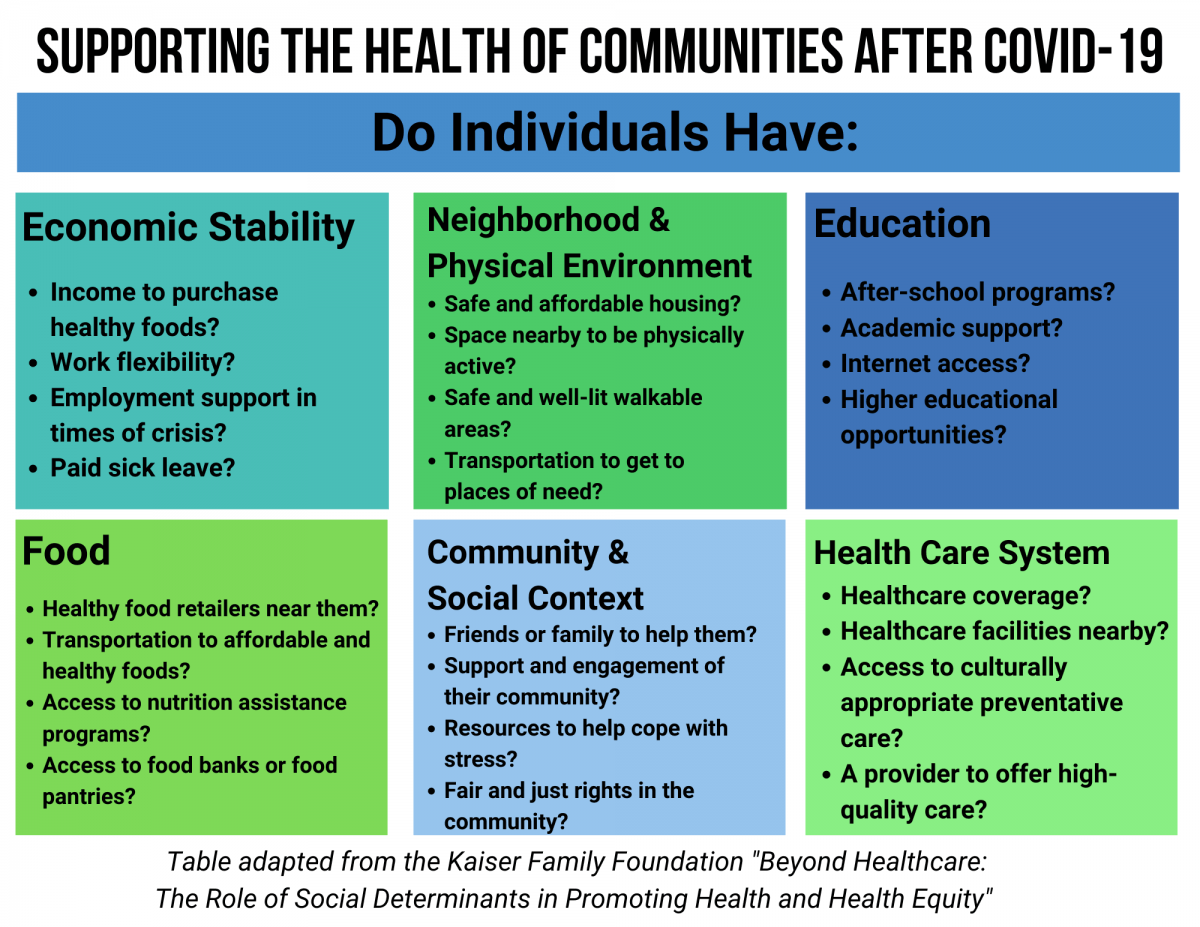
Social and economic conditions where we live, work, and play can impact our health status. These include income, affordable housing, safe places to walk, healthy food access, discrimination, and health care coverage. These conditions are connected and impact an individuals’ ability to be healthy. While Utah is typically recognized as one of the healthiest states, disparities exist that make it difficult for all Utahns to reach their full health potential.
Where do these disparities exist?
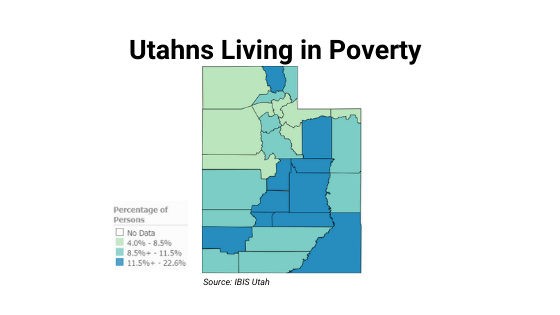
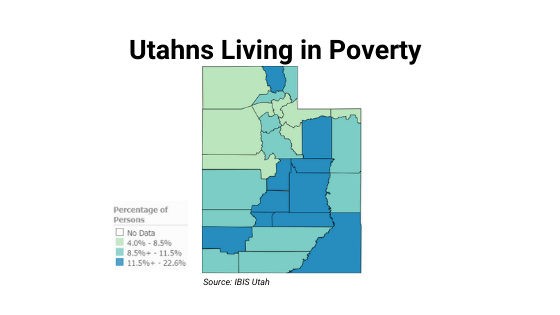
Economic Stability: Income and employment affect our ability to access healthy foods, make time for physical activity, afford medical care, find adequate housing, and manage stress. Low-income communities often have added barriers such as longer distances to healthy food and low-quality housing. In Utah, rates of poverty are higher among minority populations and individuals living in rural areas. During the COVID-19 pandemic, Hispanics have been hit particularly hard with higher unemployment rates and increased pay cuts.
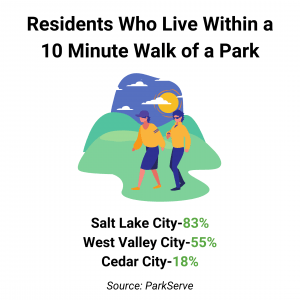
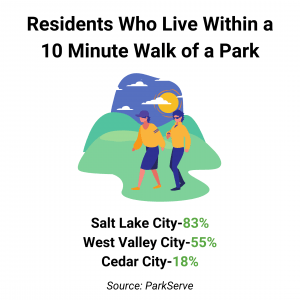
Neighborhood and Physical Environment: Our built environment, including the transportation system as well as access to parks, trails, and other outdoor spaces impacts our ability to be physically active. When individuals have safe and accessible outdoor space, they have more opportunities to be active and engaged with the community. Research also shows that those who live closer to safe sidewalks, parks, and trails are more likely to be active. At the beginning of the pandemic, Utahns started spending more time outdoors. In fact, visits to parks increased significantly. With the weather getting colder, it can be difficult for all individuals to stay active. Not all Utahns have access to indoor physical activity opportunities such as gyms and recreational facilities. Low-income and communities of color already have greater challenges accessing physical activity opportunities.
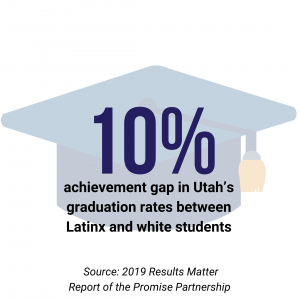
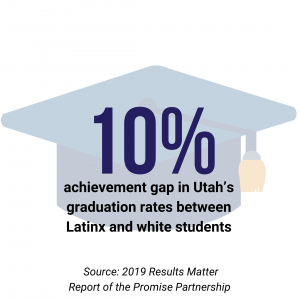
Education: Academic support and enrollment in high-quality education leads to longer lifespans, less likelihood of being exposed to violent crime, greater educational attainment, and improved economic opportunity. Utah schools are offering a variety of learning options including online, hybrid, and in-person. Social interaction for children is limited in order to help slow the spread of COVID. Low-income and families of color have disproportionately faced challenges with educational changes including managing schedule changes, finding child care, and having to stay home instead of going into work to take care of kids.
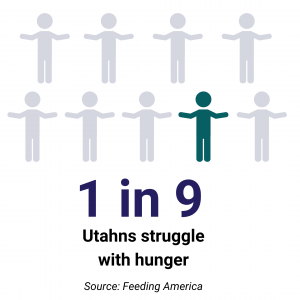
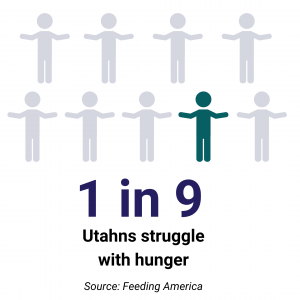
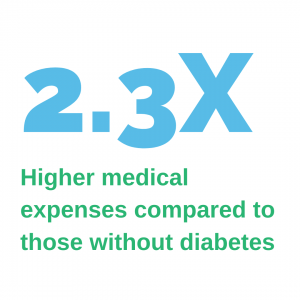
Food: Nutritious diets are linked to reduced risk of chronic diseases and improved cognitive function. Lower rates of obesity and diabetes are found in areas with increased access to healthy foods. However, many individuals do not have access to healthy food either because they cannot afford it or do not have access to a grocery store that provides healthy food options. During the COVID-19 pandemic rates of food insecurity across the country have increased. Increased unemployment rates have also led to an increased demand at food banks here in Utah.
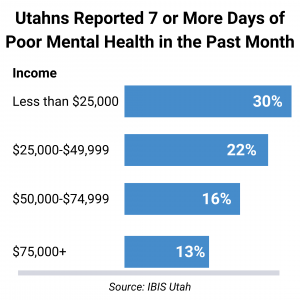
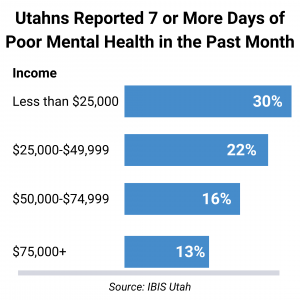
Community and Social Context: In 2018, Utah ranked 51st in a national analysis of mental health measures by Mental Health America. A number of factors impact mental health including support systems, discrimination, income, and stress. Communities with social cohesion and civic participation have more support networks, social trust, higher rates of physical activity, and reduced stress. The COVID-19 pandemic has understandably caused stress and anxiety among many individuals. Some have lost their jobs, some may be taking care of the sick family members, and many fear the unknown. Maintaining social distancing can also mean that people may feel isolated and unable to have the social support, engagement, or resources that they need.
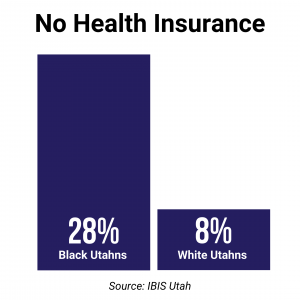
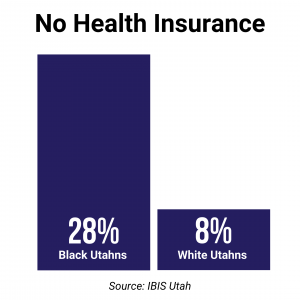
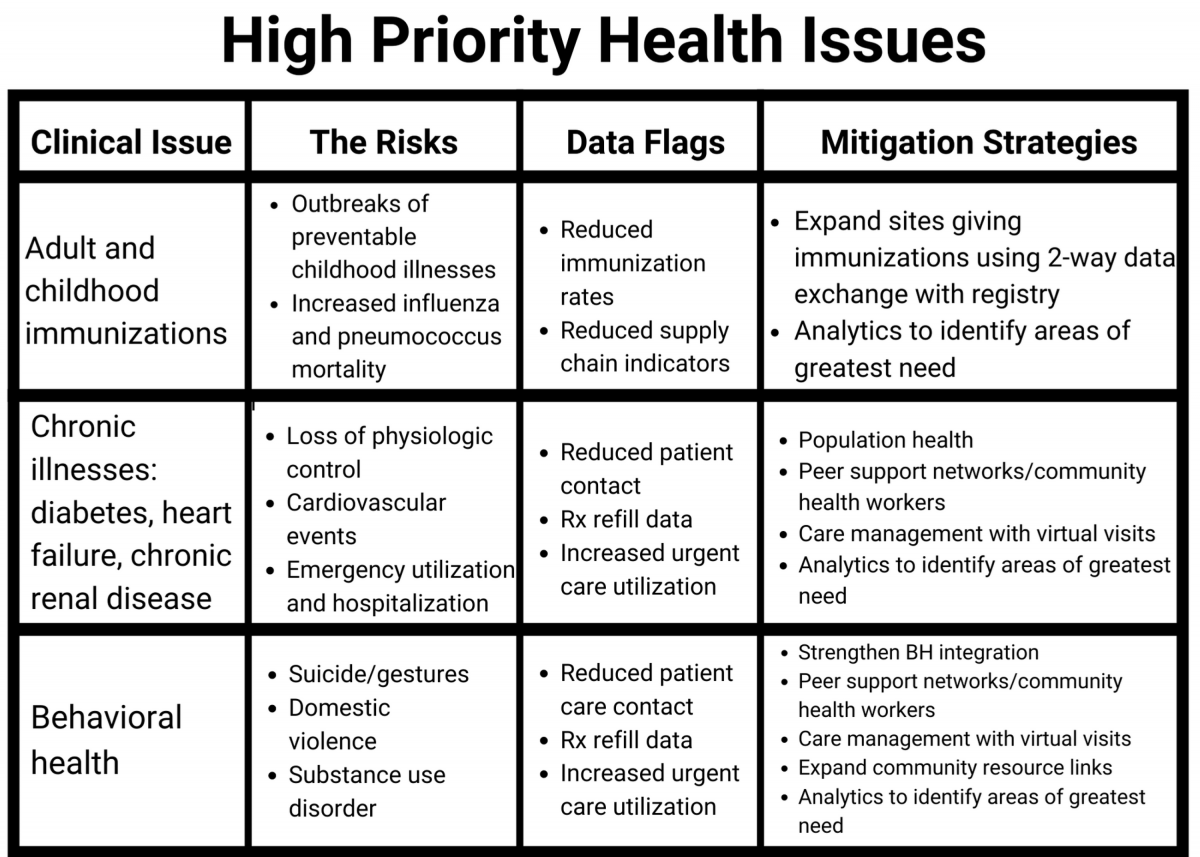
Health Care System: Access to adequate health care allows people to receive preventive screenings and appropriately manage diseases. A lack of access to a health care facilities, limited provider availability, and lack of health insurance coverage are barriers to accessing care. The COVID-19 pandemic has led to skipped or postponed medical care for nearly 50% of the population. Maintaining proper preventative care is important to reduce further health problems and reduce health care costs down the road.
Moving Forward After COVID-19
COVID-19 did not cause disparities in our communities, but rather highlighted disparities that already existed and will continue to exist. Minority populations have had disproportionately higher case rates as well as hospitalizations related to COVID-19. People with pre-existing medical conditions also have higher COVID-19 related hospitalizations and deaths.
Addressing underlying social determinants of health is critical to improving the conditions that increase the cases and severity of this pandemic. We must ensure that all Utahns have the opportunity to be healthy, now and in the future, by improving the communities where people live.
_300x220.jpg)






_300x220.jpg)



_300x220.jpg)
_300x220.jpg)



_300x220.jpg)
_300x220.jpg)


_300x220.png)

%20(1)_300x220.jpg)












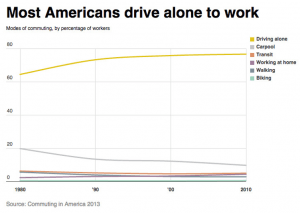 transportation both an easy choice, and a healthy choice. We are focusing on better street connectivity, protecting pedestrians and cyclists through dedicated paths, and improving the policy environment to better support these behaviors. By doing this, we are not only making our cities more connected by bringing people out of their shells (specifically their cars) but are supporting healthier lifestyles resulting in better quality of life. So, next time as you climb into your car, consider what it would take to change the way you move. Whatever you decide to do, Utah is working together to make it healthier and easier.
transportation both an easy choice, and a healthy choice. We are focusing on better street connectivity, protecting pedestrians and cyclists through dedicated paths, and improving the policy environment to better support these behaviors. By doing this, we are not only making our cities more connected by bringing people out of their shells (specifically their cars) but are supporting healthier lifestyles resulting in better quality of life. So, next time as you climb into your car, consider what it would take to change the way you move. Whatever you decide to do, Utah is working together to make it healthier and easier.
 Get Healthy Utah is proud to have partnered with
Get Healthy Utah is proud to have partnered with